Overview

Left untreated, fallen arches, or flat feet, not only cause pain but can lead to other serious foot and joint problems such as shin splints. With proper shoe selection and exercises you can begin to strengthen and restore the arches in your feet. If you are concerned about your fallen arches, consult with an experienced podiatrist.
Causes
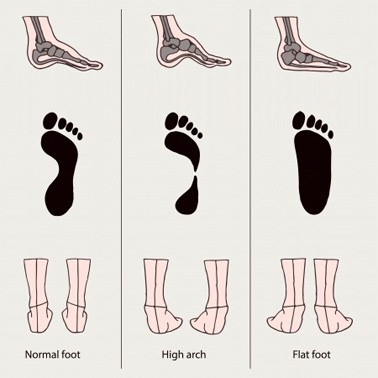
A Rigid Flat Foot may be congenital, where the arch never develops when growing. A Rigid Flat Foot can also be acquired due to disease processes involving inflammatory arthritis, neurological conditions such as Charcot neuro-arthropathy or trauma. A Flexible Flat Foot (fallen arches) may also be congenital where excessive pronation occurs for shock absorption. In some cases this condition may be the result of neurological disease or injury involving muscle weakness, hyper-mobile joints or ligament laxity. These conditions may allow for excessive pronation causing the arch to fall when weight bearing or during activity. Both of these foot types can result in posture mal-alignment involving the lower back, hips, knees and feet which may result in pain in those areas.
Symptoms
Pain and stiffness of the medial arch or anywhere along the mid-portion of the foot. Associated discomfort within and near the ankle joint. The knees, hips, and lower back may be the primary source of discomfort. Feet may often feel tired and achy. Painful shin splints may develop with activity. Gait may be awkward.
Diagnosis
If your child has flatfeet, his or her doctor will ask about any family history of flatfeet or inherited foot problems. In a person of any age, the doctor will ask about occupational and recreational activities, previous foot trauma or foot surgery and the type of shoes worn. The doctor will examine your shoes to check for signs of excessive wear. Worn shoes often provide valuable clues to gait problems and poor bone alignment. The doctor will ask you to walk barefoot to evaluate the arches of the feet, to check for out-toeing and to look for other signs of poor foot mechanics. The doctor will examine your feet for foot flexibility and range of motion and feel for any tenderness or bony abnormalities. Depending on the results of this physical examination, foot X-rays may be recommended. X-rays are always performed in a young child with rigid flatfeet and in an adult with acquired flatfeet due to trauma.
Non Surgical Treatment
There are different modalities of treatment that are available to manage flat feet and fallen arches. The type of treatment that is chosen depends upon how severe the condition is and what symptoms the patients are experiencing. Below is a brief description of the available treatment modalities. In the event that the patient is experiencing swelling of the feet, rest and ice application is usually the initial treatment step. Oral anti-inflammatories may be offered which can help reduce inflammation as well as associated pain. Physical therapy has good outcomes and can include different exercises such as stretches and strengthening of the surrounding muscles. Changes in footwear and activity modification are also important when dealing with a painful flat (pronated) foot. These days, orthotic insoles are easily available either over the counter or through your Podiatrist which can effectively help maintain the arch of the foot and reduce the amount of stress placed on the foot. Podiatrists are able to prescribe a variety of different devices from prefabricated to customized and are trained to determine the most appropriate device for each individual. In order to offer the right kind of orthotic insole, podiatrists may perform a test called gait analysis. This involves asking the patient to walk and videoing the different movements that the foot of forms during the walking. Features such as over pronation can be easily seen on this and orthotic insoles can be prescribed to correct the specific abnormalities that are picked up on this analysis. Overall, orthotic treatment can result in a significant improvement in foot movement and reduction in foot discomfort.
Surgical Treatment

Procedures may include the following. Fusing foot or ankle bones together (arthrodesis). Removing bones or bony growths, also called spurs (excision). Cutting or changing the shape of the bone (osteotomy). Cleaning the tendons' protective coverings (synovectomy). Adding tendon from other parts of your body to tendons in your foot to help balance the "pull" of the tendons and form an arch (tendon transfer). Grafting bone to your foot to make the arch rise more naturally (lateral column lengthening).
After Care
Patients may go home the day of surgery or they may require an overnight hospital stay. The leg will be placed in a splint or cast and should be kept elevated for the first two weeks. At that point, sutures are removed. A new cast or a removable boot is then placed. It is important that patients do not put any weight on the corrected foot for six to eight weeks following the operation. Patients may begin bearing weight at eight weeks and usually progress to full weightbearing by 10 to 12 weeks. For some patients, weightbearing requires additional time. After 12 weeks, patients commonly can transition to wearing a shoe. Inserts and ankle braces are often used. Physical therapy may be recommended. There are complications that relate to surgery in general. These include the risks associated with anesthesia, infection, damage to nerves and blood vessels, and bleeding or blood clots. Complications following flatfoot surgery may include wound breakdown or nonunion (incomplete healing of the bones). These complications often can be prevented with proper wound care and rehabilitation. Occasionally, patients may notice some discomfort due to prominent hardware. Removal of hardware can be done at a later time if this is an issue. The overall complication rates for flatfoot surgery are low.

Left untreated, fallen arches, or flat feet, not only cause pain but can lead to other serious foot and joint problems such as shin splints. With proper shoe selection and exercises you can begin to strengthen and restore the arches in your feet. If you are concerned about your fallen arches, consult with an experienced podiatrist.
Causes
A Rigid Flat Foot may be congenital, where the arch never develops when growing. A Rigid Flat Foot can also be acquired due to disease processes involving inflammatory arthritis, neurological conditions such as Charcot neuro-arthropathy or trauma. A Flexible Flat Foot (fallen arches) may also be congenital where excessive pronation occurs for shock absorption. In some cases this condition may be the result of neurological disease or injury involving muscle weakness, hyper-mobile joints or ligament laxity. These conditions may allow for excessive pronation causing the arch to fall when weight bearing or during activity. Both of these foot types can result in posture mal-alignment involving the lower back, hips, knees and feet which may result in pain in those areas.
Symptoms
Pain and stiffness of the medial arch or anywhere along the mid-portion of the foot. Associated discomfort within and near the ankle joint. The knees, hips, and lower back may be the primary source of discomfort. Feet may often feel tired and achy. Painful shin splints may develop with activity. Gait may be awkward.
Diagnosis
If your child has flatfeet, his or her doctor will ask about any family history of flatfeet or inherited foot problems. In a person of any age, the doctor will ask about occupational and recreational activities, previous foot trauma or foot surgery and the type of shoes worn. The doctor will examine your shoes to check for signs of excessive wear. Worn shoes often provide valuable clues to gait problems and poor bone alignment. The doctor will ask you to walk barefoot to evaluate the arches of the feet, to check for out-toeing and to look for other signs of poor foot mechanics. The doctor will examine your feet for foot flexibility and range of motion and feel for any tenderness or bony abnormalities. Depending on the results of this physical examination, foot X-rays may be recommended. X-rays are always performed in a young child with rigid flatfeet and in an adult with acquired flatfeet due to trauma.
Non Surgical Treatment
There are different modalities of treatment that are available to manage flat feet and fallen arches. The type of treatment that is chosen depends upon how severe the condition is and what symptoms the patients are experiencing. Below is a brief description of the available treatment modalities. In the event that the patient is experiencing swelling of the feet, rest and ice application is usually the initial treatment step. Oral anti-inflammatories may be offered which can help reduce inflammation as well as associated pain. Physical therapy has good outcomes and can include different exercises such as stretches and strengthening of the surrounding muscles. Changes in footwear and activity modification are also important when dealing with a painful flat (pronated) foot. These days, orthotic insoles are easily available either over the counter or through your Podiatrist which can effectively help maintain the arch of the foot and reduce the amount of stress placed on the foot. Podiatrists are able to prescribe a variety of different devices from prefabricated to customized and are trained to determine the most appropriate device for each individual. In order to offer the right kind of orthotic insole, podiatrists may perform a test called gait analysis. This involves asking the patient to walk and videoing the different movements that the foot of forms during the walking. Features such as over pronation can be easily seen on this and orthotic insoles can be prescribed to correct the specific abnormalities that are picked up on this analysis. Overall, orthotic treatment can result in a significant improvement in foot movement and reduction in foot discomfort.
Surgical Treatment

Procedures may include the following. Fusing foot or ankle bones together (arthrodesis). Removing bones or bony growths, also called spurs (excision). Cutting or changing the shape of the bone (osteotomy). Cleaning the tendons' protective coverings (synovectomy). Adding tendon from other parts of your body to tendons in your foot to help balance the "pull" of the tendons and form an arch (tendon transfer). Grafting bone to your foot to make the arch rise more naturally (lateral column lengthening).
After Care
Patients may go home the day of surgery or they may require an overnight hospital stay. The leg will be placed in a splint or cast and should be kept elevated for the first two weeks. At that point, sutures are removed. A new cast or a removable boot is then placed. It is important that patients do not put any weight on the corrected foot for six to eight weeks following the operation. Patients may begin bearing weight at eight weeks and usually progress to full weightbearing by 10 to 12 weeks. For some patients, weightbearing requires additional time. After 12 weeks, patients commonly can transition to wearing a shoe. Inserts and ankle braces are often used. Physical therapy may be recommended. There are complications that relate to surgery in general. These include the risks associated with anesthesia, infection, damage to nerves and blood vessels, and bleeding or blood clots. Complications following flatfoot surgery may include wound breakdown or nonunion (incomplete healing of the bones). These complications often can be prevented with proper wound care and rehabilitation. Occasionally, patients may notice some discomfort due to prominent hardware. Removal of hardware can be done at a later time if this is an issue. The overall complication rates for flatfoot surgery are low.









 The Achilles tendon, or calcaneal tendon, is a large ropelike band of fibrous tissue in the back of the ankle that connects the powerful calf muscles to the heel bone (calcaneus). Sometimes called the heel cord, it is the largest tendon in the human body. When the calf muscles contract, the Achilles tendon is tightened, pulling the heel. This allows you to point your foot and stand on tiptoe. It is vital to such activities as walking, running, and jumping. A complete tear through the tendon, which usually occurs about 2 inches above the heel bone, is called an Achilles tendon rupture.
The Achilles tendon, or calcaneal tendon, is a large ropelike band of fibrous tissue in the back of the ankle that connects the powerful calf muscles to the heel bone (calcaneus). Sometimes called the heel cord, it is the largest tendon in the human body. When the calf muscles contract, the Achilles tendon is tightened, pulling the heel. This allows you to point your foot and stand on tiptoe. It is vital to such activities as walking, running, and jumping. A complete tear through the tendon, which usually occurs about 2 inches above the heel bone, is called an Achilles tendon rupture.
 RSS Feed
RSS Feed